Written with contributing author Linda Robinson, MSN, CPXP, RN, Vice President of Clinical Excellence, MDM Healthcare
There are several healthcare professionals that assist families during their childbirth journey. Many families are choosing to hire doulas, trained professionals who provide physical, emotional, and informational support throughout the process. These professionals bring a lot to the table when it comes to patient experience, support that is essential for expecting parents. Debbie Young, Certified Birth and Postpartum Doula, shared some valuable insights on the topic in a recent interview.
Young explained that there are several types of doulas including traditional birth doulas, postpartum doulas, and community doulas, who serve specific communities' needs. She also noted that many hospitals do have doula programs. She elaborated on how doulas work with hospital care teams during childbirth.
“I see myself as part of a team because I am not there to do clinical things, but I am there to do the support part. You think of all the skills needed by the clinical personnel, nurse, doctor, and midwife; I want to be a part of that team. I do not replace any of them, instead, I am there as an extra bonus,” she said.
Young explained one of the things that set the role of a doula apart is that they are devoted entirely to the expecting family.
Many parents who have recently got the news they are expecting may be interested in the process of starting with a doula. Young explains that doulas meet with parents several times throughout the perinatal journey. She meets with an expecting mother at least two times and noted that the chemistry between expecting parents and their doula is important.
“First, I just to do a meet and greet for free because, as I tell families, I am going to be with you at one of the most vulnerable times of your life, and even if I am very smart, and I know what I am talking about, if I do not have a personality that matches your personality, I am not the right doula for you. Let me give you the name of a couple of other doulas in the area that you could call upon. I do stress when I talk about hiring a doula from my childbirth education classes, that parents talk to two or three people because that person is going to be at this intimate time in their lives,” she said.

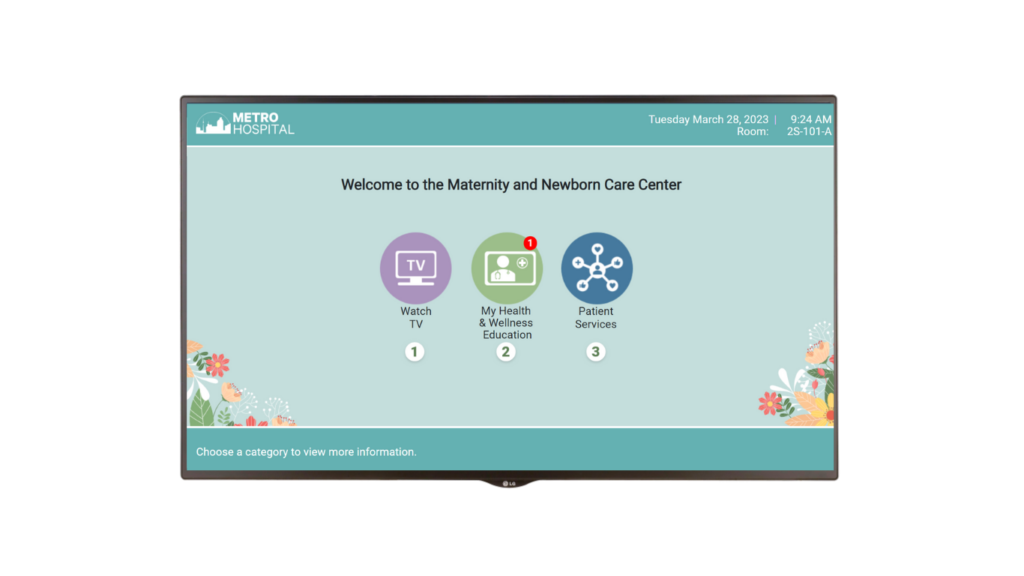
In today’s healthcare landscape care delivery models are evolving to address recent challenges such as workforce shortages. As technology continues to impact the healthcare industry, and the popularity of telehealth on the rise, many hospital organizations are beginning to invest in innovative technology tools. Journey PX Connect allows hospitals to bring an additional healthcare expert into the patient room virtually. Connect enables video calling for patients and families. The solution also provides a secure connection that allows for virtual visits and rounding by providers, nurses, other clinicians, and authorized staff, all through the patient’s in-room TV.
Linda Robinson, MSN, CPXP, RN, Vice President of Clinical Excellence, MDM Healthcare elaborated on the added value of bringing in additional experts virtually, to the bedside.
“Currently, hospitals are dealing with nurses that are overwhelmed, overworked, and an experience complexity gap. Why not look at another professional that you can add to the care team to drive quality? Technology such as Journey PX Connect provides hospitals with the ability to bring additional experts to give that added layer of support,” said Robinson.
She also noted that in specialized units like Mother Baby Units, these experts would be professionals such as doulas and lactation consultants.
The importance of education was another topic discussed by Young, who began her 35-year career in the childbirth field as a childbirth educator. Young is noted for her extensive work in childbirth education. In fact, in addition to her current role as a doula and doula trainer, she provides childbirth educational materials to health professionals, patients, and students as the Customer Relations Manager at InJoy Health Education, an education partner of Journey PX.
“Education is really important. I think that when patients go into labor just assuming everything is going to work out fine, they may have no idea what they are getting into,” said Young.
She explained that one of her most important goals is to provide expecting mothers with an education on a variety of topics that also covers a wide array of “what if” scenarios.
“When my students get into the delivery room, they are prepared. No one can be prepared for absolutely everything, but they are prepared. I just taught a class last night where we did a labor rehearsal. Next week, my class is going to be all about postpartum. Education about breastfeeding and post-birth warning signs, etc., they will need it all, and I think it is crucial,” she continued.
Providing comprehensive health education on topics such as breastfeeding, safe sleep, and post-birth warning signs is a key component of antenatal and postpartum care. The sources and delivery of this education are additional layers that impact the quality of patient care for newborns and their parents. This special environment requires a patient engagement platform that is tailored to the unique needs of new mothers, babies, and families. Recognizing this, Journey PX recently developed Journey PX Mother Baby, a new solution designed specifically for mother-baby units, which delivers vital health education, prepare parents and newborns for discharge, and enhances the overall patient experience.
To hear more from Debbie Young about the doula’s role in patient care, including assisting the nursing team and additional benefits doulas provide, listen to her full PX Space interview with host Linda Robinson, MSN, CPXP, RN, below.